Allergies: preventing the progression from atopic dermatitis to asthma
In a study published in the journal Nature Communications, scientists highlight the importance of two proteins in the progression from atopic dermatitis to allergic asthma: the cytokines TSLP and IL-1β. They also show that these two key factors may have a complementary role depending on the severity of atopic dermatitis and provide new insights into preventing the development of asthma following atopic dermatitis.
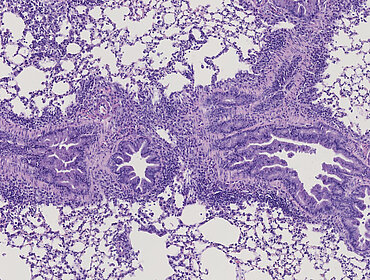
Atopic dermatitis (AD) is an inflammatory skin disease that affects 20% of children and 3% of adults. It usually begins around 3 months of age in newborns and often precedes other atopic diseases, such as asthma, in a process called atopic march. Since current treatments decrease symptoms without curing asthma, there is a need to identify strategies to stop the atopic march.
Allergic asthma develops in two phases: a sensitization phase and a revelation phase. Allergic sensitization can occur through the skin of patients with AD because it has a defective skin barrier and an inflammatory microenvironment that facilitates its development. Due to the complexity and heterogeneity of AD, the way this microenvironment regulates cutaneous allergic sensitization and the atopic course remains poorly understood to date. The severity of AD can lead to allergen exposure at different skin depths and thus involve different inflammatory microenvironments, which remain difficult to study due to the lack of relevant experimental systems.
In this study, scientists develop an experimental system to induce allergic sensitization during mild atopic dermatitis (through the epidermis, epicutaneous sensitization) or during severe atopic dermatitis (through the dermis, dermacutaneous sensitization) in mice. The authors show that targeting the cytokine TSLP, produced by epithelial cells, during epicutaneous sensitization is sufficient to prevent the atopic march. On the contrary, TSLP has only a partial role in dermacutaneous sensitization, while IL-1β, another cytokine produced by immune cells infiltrating atopic dermatitis lesions, plays a complementary role in promoting allergic sensitization and progression to asthma. This study identifies TSLP and IL-1β as two key factors involved in cutaneous allergic sensitization and atopic gait, and that their role depends on the context of sensitization.
This work provides new insights regarding the development of biological targets to stop atopic walking, and reinforces the importance of personalized targets to achieve better efficacy.
